The Silent Emergency: Inside Kano’s Maternal Mortality Crisis
Nafisa Salahu’s labor lasted three days. As contractions ripped through her body, the understaffed Kano clinic could only advise her to “lie still.” No doctor assessed her obstructed labor. When a surgeon finally performed an emergency cesarean, her baby was dead. “I was almost dying,” she recalls. “I had no strength left.” Nafisa survived, but Nigeria loses one mother every seven minutes—the highest maternal death rate globally. In Kano alone, eight recent deaths exposed a brutal truth: clinics lack staff, equipment, and hope.
The Data of Despair: Nigeria’s Deadly Leadership
Nigeria accounts for 29% of global maternal deaths—75,000 women annually. In Kano, a woman faces a 1 in 25 lifetime risk of maternal death, compared to 1 in 5,900 in Spain. The causes are infuriatingly preventable:
- Postpartum hemorrhage (37%): Clinics lack blood banks and tranexamic acid.
- Obstructed labor: No surgical capacity for emergency C-sections.
- Hypertensive disorders: Absent blood pressure monitors and magnesium sulfate.
| Location | Key Deficits | Lifetime Risk |
|---|---|---|
| Kano State | No blood banks; midwife shortages | 1 in 25 |
| Jigawa State | No incubators; antibiotic stockouts | Under-5 mortality: 161/1,000 |
| Rural Clinics | 60% lack functional BP monitors | 1.5x urban MMR |
Conflict zones compound the crisis: maternal deaths are five times higher in areas like Northern Nigeria than in stable regions.
Anatomy of a Crisis: Staff, Supplies, and Systemic Failure
Staffing Shortages: Clinics Running on Empty
Kano’s clinics operate with skeleton crews. Nigeria has only 121,000 midwives for 218 million people—far below minimum recommendations. A damning study revealed only 16% of birth attendants can manage postpartum hemorrhage. Health workers average less than 46% competency scores in emergency obstetric care. Doctors flee to cities or abroad, leaving rural clinics with locum staff untrained in life-saving procedures.
Equipment Graveyards
Walk into a typical Kano clinic, and you’ll find no PPH kits (oxytocin and compression sutures absent in 80% of facilities), empty blood banks (screening kits and refrigeration unavailable), and broken fetal monitors critical for detecting fetal distress. During health emergencies, testing was suspended due to reagent shortages—health workers rationed face masks as protective equipment.
The Three Deadly Delays
- Decision to seek care: Cultural distrust persists. Jamila Ishaq, a mother of five, avoids hospitals after neglect during labor: “No healthcare worker was available to help me.”
- Reaching facilities: Isolation centers are overwhelmed; rural roads lack ambulances.
- Receiving treatment: Drug stockouts and 6-hour waits plague facilities.
Roots of Neglect: Funding, Data, and Gender Injustice
Chronic underfunding sees Nigeria spending only 5% of its budget on health—below the 15% African Union target. Hiring freezes cripple staffing. Data darkness persists with limited tracking of maternal deaths. The Maternal Mortality Reduction Innovation Initiative (Mamii) aims to link 400,000 pregnant women to care but operates in only six states. Gender inequality remains stark: child marriage and low female education restrict health autonomy. Over 60% of rural women deliver without skilled attendants.
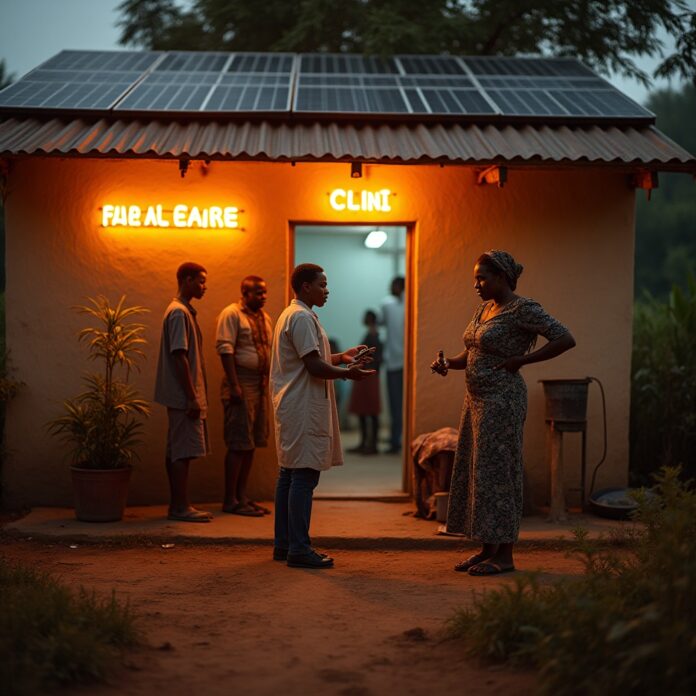
Pathways to Hope: Solutions in Action
State and Federal Initiatives
Kano launched a Social and Behaviour Change Communication strategy in June 2025, mobilizing traditional leaders and media to boost health-seeking behaviors. Funded by international partners, it deploys community dialogues and digital outreach. The Mamii Program conducts house-to-house pregnancy tracking and provides transport vouchers to combat the “first delay.” A free maternity project offers free caesarean sections and delivery kits at state facilities.
Global Partnerships
International initiatives target midwifery training and supply chains in high-risk zones like Kano. Specific programs train birth attendants on postpartum hemorrhage protocols—critical when hemorrhage causes 37% of deaths. Governor Abba Kabir Yusuf pledged to significantly reduce maternal mortality by June 2025, describing it as a top priority.
| Initiative | Key Actions | Potential Impact |
|---|---|---|
| Midwifery Model of Care | Train 10,000 midwives; deploy to local areas | Reduce hemorrhage deaths by 50% |
| Tertiary Health Insurance | Integrate clinics into state insurance | End drug stockouts |
| Mobile Clinics | Units with surgical capacity | Cut rural mortality by 30% |
Call to Action: No More Nafisas
- EQUIP every clinic with emergency obstetric kits: hemorrhage medications, anticonvulsants, vacuum extractors.
- TRAIN 20,000 midwives in hemorrhage control by 2026.
- FUND health at 15% of budgets—audit allocations transparently.
- AMPLIFY community voices: Women like Jamila must shape policies.
“No woman deserves to die while birthing a child.” Yet in Kano, childbirth remains a lethal gamble. The deficit isn’t just clinical—it’s a moral collapse. Fixing it demands more than temporary solutions; it requires a revolution.
Epilogue: The Faint Pulse of Progress
Kano’s communication strategy and Mamii program signal awareness, but execution is non-negotiable. Maternal health is a right, not a privilege. With 75,000 Nigerian mothers dying yearly, half-measures are complicity. Invest in emergency obstetric care, and we don’t just save mothers—we resurrect hope.