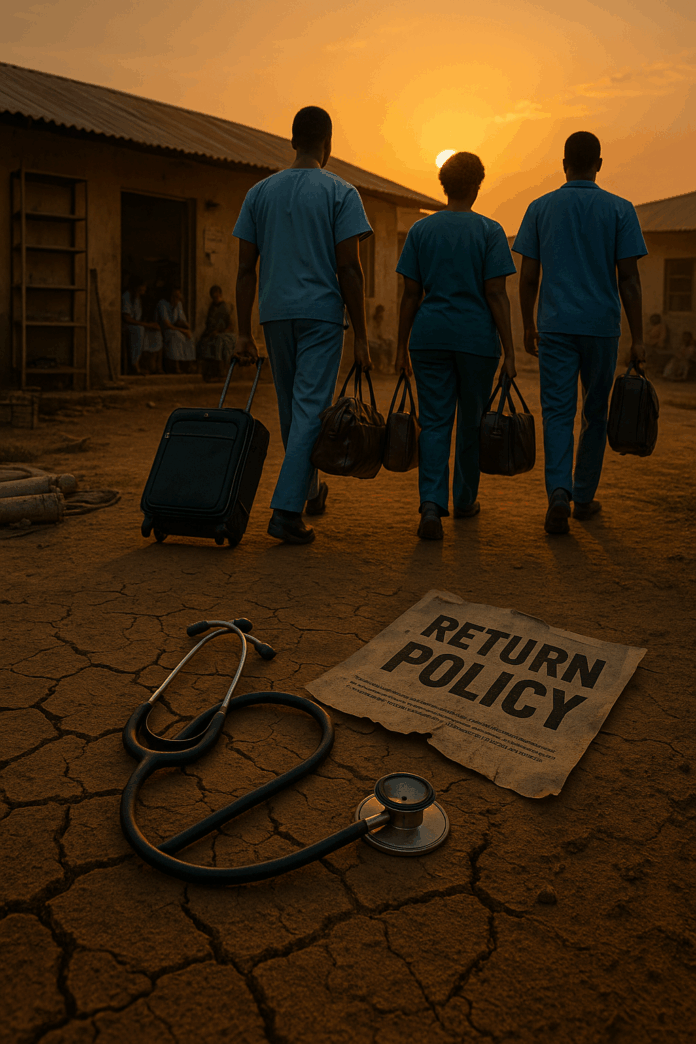
The Paradox of Flight Amidst Calls for Return
Let’s start with a number that should shake us all: 5,000. That’s how many physicians have packed their stethoscopes and left developing nations just in the first half of 2025. Think about it—entire towns, regions, and vulnerable populations stripped of their lifelines. And here’s the cruel irony: while destination countries like the UK roll out red carpets with specialized visas (like the Health and Care Visa), and origin nations desperately negotiate “bilateral return agreements,” health workers keep voting with their feet. Why? Because policy papers don’t heal burnout, pay rent, or replace broken elevators that kill colleagues.
Governor Muthomi Njuki of Kenya’s Council of Governors put it bluntly: “We’re giving away the crème de la crème while struggling to employ them. Exporting health workers steals our future.” This isn’t just “brain drain”—it’s brain drain persistence: a vicious cycle where systemic neglect and hollow promises overpower short-term fixes. The heart wants to serve home, but home won’t provide gloves, living wages, or safety.
Global Triage: Mapping the 2025 Health Worker Exodus
Africa’s Accelerating Crisis
Kenya: 64.4% of health professionals actively seek emigration. The country trains over 600 new doctors annually but can’t absorb them. Doctor density? A grim 14 per 100,000 people—far below WHO’s 21.7 minimum.
Ghana: Loses ~500 nurses monthly to the West. The UK now employs more Ghanaian nurses than Ghana itself.
Nigeria: Over 9,000 doctors fled between 2016–2018. By 2025, projections warn of losing 50% of skilled health workers. Lagos University Teaching Hospital recently shuttered 150 beds due to staff shortages.
Zimbabwe: Doctors earn $100–$150/month amid PPE shortages. Over 4,000 health workers left in 2021–2022 alone. By 2025, the UK had issued 21,130 work visas to Zimbabweans—many for care roles.
Western Systems in Peril
United States: The public health workforce shrunk 46% from 2017–2021. Burnout and harassment during COVID-19 drove 75% of young workers to consider exiting.
Canada: Nursing unions battle retention as 75% of clinicians globally plan to leave healthcare by 2025. Why? Crushing workloads and emotional trauma.
The “Greener Pastures” Calculus
It’s not greed—it’s survival.
Table: Salary Disparities Driving Exodus (2025)
| Country/Region | Doctor Monthly Salary | Nurse Monthly Salary | Key Destination | Destination Salary |
|---|---|---|---|---|
| Ghana | $400–$600 | $150–$300 | United Kingdom | $4,000–$6,000 |
| Zimbabwe | $100–$150 | $50–$75 | Saudi Arabia | $2,140–$6,000 |
| Kenya | $500–$800 | $300–$500 | Germany | $5,000–$8,000 |
A Zimbabwean nurse’s lament: “I couldn’t afford basics. Sometimes you don’t have gloves to work with. In the UK, things are totally different.”
Why “Return Policies” Are Failing: Systemic Roots of Persistence
The False Promise of Bilateral Agreements
Kenya signed a deal with the UK in 2021 to “manage migration.” By 2024, 280 nurses had left for Britain. How many returned? Near zero. The UK’s “red list” bans recruitment from 55 vulnerable countries, but private agencies exploit loopholes, stripping nations like Zimbabwe of seasoned professionals.
Unaddressed Push Factors
Underfunding: Only Mauritius, Seychelles, and Eritrea meet the AU’s pledge to allocate 15% of budgets to healthcare. Nigeria spends just 3.9%.
Workplace Trauma: 75% of U.S. public health workers faced harassment or threats during COVID-19. In Zimbabwe, nurses strike over lack of PPE and $75/month salaries.
Professional Stagnation: Kenyan nurses cite outdated tech and skills decay. As one director noted: “Recruiting countries select the most experienced. Novices are left without guidance.”
The Digital Nomad Effect
Telehealth and global licensure (e.g., Canada’s proposed national framework) let doctors serve foreign systems remotely—without ever coming home. Why return to surgery by candlelight when you can consult from a safe desk?
The Domino Effect: How Brain Drain Sabotages Health Systems
Collapse in Care Quality
Liberia’s 0.1 doctors/1,000 people force nurses to handle complex cases far beyond their training.
In Kenya, the exodus of experienced nurses leaves novices unsupervised, increasing medical errors.
Zimbabwe’s HIV/TB programs—once success stories—now flounder as nurses driving treatment adherence emigrate.
Economic False Economy
Kenya celebrates $1.7B in remittances funding factories, but loses $100M+ training doctors who emigrate.
U.S. hospitals hemorrhage cash, spending $100K+/nurse on temporary staff to plug burnout-induced gaps.
The Silent Epidemics
Life expectancy in Zimbabwe dropped to 58.5 years—below Africa’s average of 63.6. Preventable killers like HIV, respiratory infections, and neonatal conditions surge as staff vanish.
Beyond Toothless Policies: Innovations That Could Stem the Tide
Ethical Destination Engagement
Skills Bonds: UK/Germany could fund Kenyan rural clinics for each nurse recruited—offsetting loss with direct investment.
Diaspora Knowledge Networks: Kenya’s proposed virtual mentorship lets emigrant doctors upskill home teams without physical return.
Origin Country Reforms
Radical Wage Parity: Ghana pilots 200% salary hikes for rural specialists via World Bank loans.
Scope-of-Practice Revolution: Canada’s 2025 mandates equal pay for nurse practitioners, retaining critical primary care roles.
Mental Health Shields: U.S. loan repayment programs for public health grads who stay in government roles combat trauma-driven exits.
Data-Driven Accountability
WHO’s Support and Safeguards List tracks 55 critical-shortage countries to target aid.
Canada’s “unique nurse identifier” monitors real-time attrition—triggering interventions before wards close.
Table: Return Policy Promises vs. 2025 Realities
| Policy Approach | Promise | 2025 Reality | Gap |
|---|---|---|---|
| Bilateral Labor Pacts (e.g., Kenya-UK) | Managed migration + return incentives | 280 nurses sent to UK; near-zero return | No penalty for non-return; home conditions unchanged |
| “Health Worker Visa” (UK) | Ethical recruitment | Private agencies recruit from red-list nations | Weak enforcement; profit-driven recruitment |
| Mental Health Support (U.S./Canada) | Reduce burnout exits | 75% healthcare workers plan to quit | Underfunded; culture change lacking |
Breaking the Cycle – It’s About Justice, Not Just Jobs
We stand at a 2025 inflection point: 129,000+ health workers will exit globally this year. Systems in Nigeria, Kenya, and beyond teeter on collapse. Return policies? They’re bandages on bullet wounds.
The solution isn’t guilt-tripping doctors into martyrdom. It’s brain equity: demanding destination countries invest in source-nation health systems as ethical reciprocity. It’s Kenya’s nurses owning shifts they design. It’s Zimbabwean surgeons earning enough to fix elevators before they kill colleagues.
Setfree Mafukidze, a Zimbabwean nurse in Somerset, said it best: “The heart belongs home. But home doesn’t provide the tools for the trade. Or mental care for its workers.”
Until policies honor that truth—until safety, living wages, and dignity anchor every clinic—no visa deal or “return framework” will heal this hemorrhage. Because you can’t rebuild a health system with empty promises and empty scrubs.