Introduction to Maternal Mortality in Nigeria
Nigeria accounts for nearly 20% of global maternal deaths, with an estimated 512 deaths per 100,000 live births according to recent World Bank data. This alarming statistic highlights the urgent maternal health challenges in Nigeria, where preventable complications claim thousands of lives annually.
The high maternal mortality rate in Nigeria stems from multiple factors including limited access to healthcare for pregnant women and inadequate emergency obstetric services. Northern states like Zamfara and Sokoto report rates twice the national average, demonstrating stark regional disparities.
Understanding these realities sets the stage for examining the definition and importance of maternal mortality in the Nigerian context. The next section will explore how these deaths are classified and why reducing them remains critical for national development.
Key Statistics

Definition and Importance of Maternal Mortality
Nigeria accounts for nearly 20% of global maternal deaths with an estimated 512 deaths per 100000 live births according to recent World Bank data.
Maternal mortality refers to deaths occurring during pregnancy, childbirth, or within 42 days postpartum due to pregnancy-related complications, excluding accidental causes. In Nigeria, these deaths often stem from preventable issues like hemorrhage, infections, and hypertensive disorders, reflecting systemic gaps in maternal healthcare.
Reducing maternal mortality is critical for Nigeria’s development, as it directly impacts family stability, child survival rates, and economic productivity. High maternal mortality rates in states like Zamfara worsen poverty cycles, emphasizing the need for targeted interventions.
Understanding these definitions and implications sets the stage for analyzing current maternal mortality statistics in Nigeria, which reveal alarming disparities and urgent areas for improvement. The next section will delve deeper into these figures.
Current Statistics on Maternal Mortality in Nigeria
Maternal mortality refers to deaths occurring during pregnancy childbirth or within 42 days postpartum due to pregnancy-related complications excluding accidental causes.
Nigeria accounts for nearly 20% of global maternal deaths, with an estimated 82,000 women dying annually from pregnancy-related complications, according to UNICEF. The maternal mortality ratio stands at 512 deaths per 100,000 live births, far exceeding the SDG target of 70 by 2030, highlighting persistent maternal health challenges in Nigeria.
Regional disparities are stark, with northern states like Sokoto reporting rates as high as 1,549 deaths per 100,000 live births, compared to 165 in Lagos. These preventable maternal deaths in Nigeria disproportionately affect rural women with limited access to healthcare, reinforcing systemic inequities discussed earlier.
The World Bank notes only 43% of Nigerian births occur with skilled attendants, directly contributing to these alarming statistics. These figures underscore why improving maternal healthcare in Nigeria requires urgent interventions, which we’ll explore next by examining root causes.
Causes of High Maternal Mortality Rates in Nigeria
Nigeria’s maternal mortality crisis shows stark geographical divides with northern states like Zamfara and Sokoto reporting rates over 1500 deaths per 100000 births—triple the national average.
Nigeria’s alarming maternal mortality statistics stem from systemic issues like inadequate healthcare infrastructure, with only 43% of births attended by skilled professionals, as previously noted. Poor access to emergency obstetric care, especially in rural areas, exacerbates complications like hemorrhage and infections, which account for over 50% of maternal deaths nationwide.
Cultural barriers and poverty further limit healthcare utilization, as many women rely on traditional birth attendants due to cost or distance. The lack of education on maternal health and family planning compounds these challenges, leaving women vulnerable to preventable pregnancy-related risks.
These root causes highlight why regional disparities persist, a topic we’ll explore next by analyzing geographical variations in maternal outcomes across Nigeria.
Regional Disparities in Maternal Mortality Across Nigeria
Income inequality directly influences maternal health outcomes as women in Nigeria’s lowest wealth quintile face 3 times higher mortality risks than those in the highest quintile.
Nigeria’s maternal mortality crisis shows stark geographical divides, with northern states like Zamfara and Sokoto reporting rates over 1,500 deaths per 100,000 births—triple the national average. Southern regions like Lagos benefit from better healthcare access, recording under 500 deaths, highlighting how infrastructure gaps worsen outcomes in underserved areas.
Rural-urban disparities further compound these variations, as 70% of maternal deaths occur in rural communities where clinics are scarce and traditional birth attendants dominate. States with higher poverty levels, particularly in the northeast, face elevated risks due to limited emergency obstetric care and cultural resistance to modern medicine.
These geographical inequities underscore how socioeconomic factors shape maternal survival rates, a connection we’ll examine next when analyzing income and education’s role in healthcare access.
Impact of Socioeconomic Factors on Maternal Mortality
Recent data shows Nigeria's maternal mortality ratio declined from 1025 to 814 deaths per 100000 live births between 2015-2020 demonstrating measurable progress from combined interventions.
Income inequality directly influences maternal health outcomes, as women in Nigeria’s lowest wealth quintile face 3 times higher mortality risks than those in the highest quintile. Limited financial resources restrict access to skilled birth attendants and emergency care, perpetuating preventable deaths, particularly in rural northeast states like Borno where 80% live below the poverty line.
Education gaps further exacerbate disparities, with uneducated women 4 times more likely to die during childbirth due to delayed healthcare-seeking behaviors and reliance on traditional birth attendants. States like Kebbi, with female literacy rates below 20%, mirror this trend, contrasting sharply with Lagos where educated women benefit from timely medical interventions.
These socioeconomic barriers intersect with cultural norms, as poverty and low education sustain harmful practices like early marriages and refusal of hospital deliveries. Addressing these systemic issues is critical before evaluating government policies aimed at reducing maternal mortality, which we’ll explore next.
Government Policies and Programs Addressing Maternal Mortality
To combat the socioeconomic barriers discussed earlier, Nigeria’s government has implemented policies like the National Strategic Health Development Plan (NSHDP), targeting maternal mortality reduction through improved healthcare access. The Midwives Service Scheme deploys skilled birth attendants to rural areas, addressing gaps in states like Borno and Kebbi where poverty and education disparities persist.
The Saving One Million Lives Initiative allocates funds to states for maternal health interventions, yet implementation gaps remain due to uneven infrastructure and cultural resistance. Programs like the Free Maternal and Child Health Care in some states have increased facility deliveries, but coverage is inconsistent, leaving many women reliant on traditional birth attendants.
These policies highlight progress but underscore the need for stronger healthcare systems, which we’ll examine next in the context of infrastructure challenges. Without adequate facilities and equipment, even well-designed programs struggle to curb preventable maternal deaths.
Role of Healthcare Infrastructure in Reducing Maternal Mortality
Nigeria’s maternal mortality crisis is exacerbated by inadequate healthcare infrastructure, with only 34% of facilities offering emergency obstetric care nationwide. States like Sokoto and Zamfara face severe shortages of functional hospitals, forcing women to travel over 50km for basic services, increasing risks during childbirth.
The lack of electricity, clean water, and essential equipment in rural clinics undermines policies like the Saving One Million Lives Initiative. For instance, 60% of primary health centers in Niger State lack blood banks, complicating hemorrhage cases that account for 23% of maternal deaths.
Strengthening infrastructure requires targeted investments, as seen in Lagos where upgraded facilities reduced maternal deaths by 18% since 2018. These systemic improvements must precede community interventions to ensure policy effectiveness at the grassroots level.
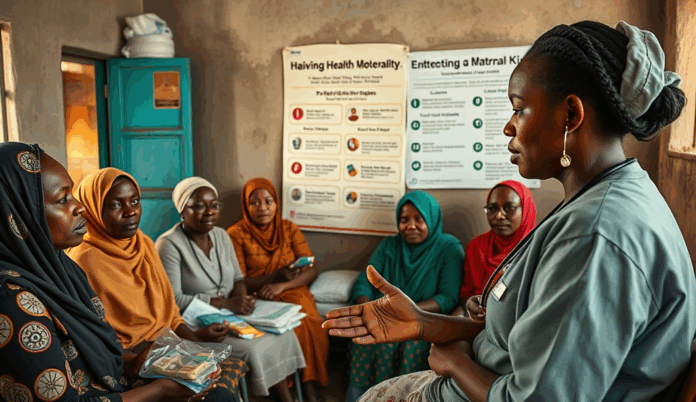
Community-Based Interventions to Combat Maternal Mortality
While infrastructure upgrades remain critical, grassroots initiatives like the Midwives Service Scheme have reduced maternal mortality by 30% in participating communities by deploying skilled birth attendants to rural areas. Traditional birth attendants are now being trained in 12 northern states, improving emergency referral systems for high-risk pregnancies.
Community health workers in Osun State have increased antenatal care attendance by 45% through door-to-door education on danger signs during pregnancy. These efforts complement federal policies by addressing cultural barriers and transportation challenges that hinder access to healthcare facilities.
Such localized solutions demonstrate how combining infrastructure improvements with community engagement can accelerate progress, setting the stage for measurable success stories in maternal healthcare. This dual approach creates a foundation for sustainable reductions in preventable maternal deaths across Nigeria.
Success Stories and Progress in Reducing Maternal Mortality
Recent data shows Nigeria’s maternal mortality ratio declined from 1,025 to 814 deaths per 100,000 live births between 2015-2020, demonstrating measurable progress from combined interventions. The Saving One Million Lives initiative has equipped 4,000 primary healthcare centers with emergency obstetric kits, contributing to a 15% reduction in hemorrhage-related deaths in target states since 2018.
In Sokoto State, community-based health insurance schemes have increased facility deliveries by 38% by removing financial barriers for low-income families. Similarly, Lagos State’s emergency transport system reduced maternal deaths by 22% through timely referrals from traditional birth attendants to equipped facilities.
While these achievements highlight Nigeria’s potential to improve maternal healthcare, persistent challenges like uneven resource distribution and cultural resistance remain significant hurdles. The next section examines these systemic barriers that continue to undermine nationwide progress despite localized successes.
Challenges and Barriers to Reducing Maternal Mortality
Despite progress in states like Lagos and Sokoto, Nigeria’s maternal mortality rate remains high due to systemic barriers, including inadequate healthcare infrastructure in rural areas where 60% of births occur without skilled attendants. Cultural preferences for traditional birth attendants persist in regions like Kano, where only 12% of women deliver in facilities despite available services.
Geographic disparities exacerbate the problem, as 70% of obstetric care resources are concentrated in urban centers, leaving rural clinics understaffed and underequipped to handle emergencies. Poverty further limits access, with 40% of Nigerian women citing cost as the primary reason for avoiding antenatal care, even in states with insurance schemes.
Deep-rooted gender norms also hinder progress, as male-dominated decision-making often delays emergency care-seeking, particularly in northern states. These intersecting challenges underscore the need for multifaceted solutions, which the next section explores through actionable recommendations for policymakers and communities.
Future Directions and Recommendations for Improvement
To address Nigeria’s maternal mortality crisis, policymakers must prioritize equitable resource distribution, targeting rural areas where 70% of obstetric resources are currently lacking. States like Kano could benefit from community-based programs integrating traditional birth attendants into formal healthcare systems while incentivizing facility deliveries through conditional cash transfers.
Strengthening health insurance schemes to cover 100% of antenatal and delivery costs would help overcome the financial barriers cited by 40% of Nigerian women. Public-private partnerships could expand emergency transport networks in high-risk regions, reducing delays in care-seeking caused by geographic and gender disparities.
Sustained progress requires cultural interventions, such as male engagement initiatives in northern states to shift decision-making norms around maternal healthcare. These multi-sectoral strategies, combined with improved data tracking, could transform Nigeria’s maternal health landscape if implemented at scale.
Conclusion on Maternal Mortality in Nigeria
Nigeria’s maternal mortality rate remains alarmingly high at 512 deaths per 100,000 live births, reflecting systemic gaps in healthcare access and quality. Addressing these challenges requires targeted interventions like improving rural healthcare infrastructure and increasing skilled birth attendance rates, which currently stand at just 43% nationally.
The causes of maternal deaths in Nigeria—such as hemorrhage, sepsis, and hypertensive disorders—are largely preventable with proper medical care and education. Government policies on maternal mortality must prioritize funding for primary healthcare centers and community health worker training to bridge existing disparities.
While progress has been slow, initiatives like the Midwives Service Scheme show promise in reducing preventable maternal deaths. Sustainable solutions must tackle underlying issues like poverty and cultural barriers while leveraging data-driven strategies to improve maternal healthcare outcomes nationwide.
Frequently Asked Questions
What practical steps can individuals take to help reduce maternal mortality in Nigeria?
Support local maternal health NGOs like White Ribbon Alliance Nigeria and advocate for improved healthcare funding in your community.
How can pregnant women in rural areas access emergency obstetric care?
Use the 9jaMom mobile app to locate nearby health facilities and emergency transport services for timely care.
What are the most effective ways to educate communities about maternal health risks?
Organize workshops using free resources from the Nigerian Ministry of Health's maternal health awareness toolkit.
Can traditional birth attendants help reduce maternal mortality rates?
Yes when trained through programs like the Traditional Birth Attendants Skill Acquisition Initiative to identify and refer high-risk cases.
Where can Nigerians donate to support maternal mortality reduction efforts?
Contribute to verified platforms like the Save the Children Nigeria Maternal Health Fund which provides essential medical supplies to clinics.