Introduction to Lassa Fever Outbreak in Nigeria
Lassa fever, an acute viral hemorrhagic illness, remains a persistent public health challenge in Nigeria, with annual outbreaks reported since its first identification in 1969. The disease, endemic in several states including Edo, Ondo, and Bauchi, peaks during the dry season (November-April) when rodent-to-human transmission increases due to environmental factors.
Healthcare professionals face unique challenges in managing Lassa fever cases, given its nonspecific early symptoms resembling malaria or typhoid. Recent data from the Nigeria Centre for Disease Control (NCDC) shows case fatality rates exceeding 20% in some outbreaks, underscoring the need for heightened vigilance.
Understanding transmission dynamics and risk factors is critical for effective outbreak response, as we’ll explore in the next section on current statistics. The disease’s zoonotic nature, primarily spread by Mastomys natalensis rodents, complicates containment efforts in rural and urban Nigerian communities.
Key Statistics

Current Statistics and Trends of Lassa Fever in Nigeria
Early-stage Lassa fever symptoms mimic common febrile illnesses with 80% of cases presenting with gradual-onset fever general weakness and headache—often leading to misdiagnosis in Nigeria’s high-burden states.
The NCDC reported 4,654 suspected Lassa fever cases and 857 confirmed cases in 2023, with a case fatality rate of 18.5%, highlighting persistent transmission risks despite containment efforts. Edo, Ondo, and Bauchi states accounted for 72% of confirmed cases, aligning with historical patterns of endemic spread during peak dry seasons.
Healthcare facilities recorded a 15% increase in Lassa fever cases compared to 2022, with late presentation and misdiagnosis contributing to higher mortality rates in rural communities. Improved surveillance has led to earlier detection, yet challenges remain in differentiating early symptoms from malaria and typhoid in primary care settings.
These trends underscore the need for targeted interventions, particularly in high-burden states, as we examine geographical hotspots in the next section. The zoonotic transmission cycle continues to drive outbreaks, necessitating integrated rodent control and community awareness programs.
Geographical Spread and Hotspots of Lassa Fever in Nigeria
Given the nonspecific early symptoms rapid laboratory confirmation is critical with reverse transcription-polymerase chain reaction (RT-PCR) being the gold standard for detecting Lassa virus RNA within 7 days of symptom onset.
Edo, Ondo, and Bauchi states remain Nigeria’s Lassa fever epicenters, accounting for 72% of confirmed cases in 2023 due to persistent rodent-to-human transmission and healthcare infrastructure gaps. Secondary hotspots include Taraba, Ebonyi, and Plateau states, where seasonal outbreaks correlate with agricultural activities and poor food storage practices in rural communities.
The disease follows distinct geographical patterns, with southern states showing year-round transmission and northern states experiencing peak outbreaks during December-April dry seasons when rodent populations invade homes. Cross-border spread from neighboring Benin and Niger remains a concern, particularly in border communities with limited health surveillance capacity.
Understanding these spatial patterns informs targeted interventions, as we’ll explore next how symptom recognition can improve early detection in these high-risk zones. The zoonotic nature of transmission underscores why hotspot mapping must integrate both human case data and rodent population dynamics.
Symptoms and Clinical Presentation of Lassa Fever
Following confirmed diagnosis through RT-PCR or ELISA immediate initiation of ribavirin therapy remains the cornerstone of Lassa fever treatment particularly when administered within 6 days of symptom onset to reduce mortality from 50% to 15%.
Early-stage Lassa fever symptoms mimic common febrile illnesses, with 80% of cases presenting with gradual-onset fever, general weakness, and headache—often leading to misdiagnosis in Nigeria’s high-burden states. Gastrointestinal symptoms like nausea, vomiting, and diarrhea frequently appear within 3-5 days, particularly in cases linked to rodent-contaminated food storage in rural hotspots.
Severe cases progress to hemorrhagic manifestations (gum bleeding, epistaxis) and neurological symptoms (tremors, hearing loss), with case fatality reaching 15-20% when treatment delays occur—common in areas with healthcare infrastructure gaps. Pregnant women in third trimester face 30% mortality risk, underscoring the urgency of symptom recognition during seasonal outbreaks in northern dry seasons.
Differentiating Lassa fever from malaria or typhoid requires vigilance in endemic zones, as we’ll explore in diagnostic methods. The nonspecific early presentation demands heightened suspicion in patients from Edo, Ondo, or Bauchi—states accounting for 72% of Nigeria’s confirmed cases.
Diagnostic Methods for Lassa Fever in Healthcare Settings
Healthcare professionals must bridge hospital protocols with community action adapting NCDC's color-coded waste segregation principles into household rodent control messaging particularly in endemic states like Edo and Ondo where 68% of 2023 cases originated.
Given the nonspecific early symptoms, rapid laboratory confirmation is critical, with reverse transcription-polymerase chain reaction (RT-PCR) being the gold standard for detecting Lassa virus RNA within 7 days of symptom onset. In Nigeria’s tertiary hospitals like Irrua Specialist Teaching Hospital, ELISA testing for IgM and IgG antibodies complements RT-PCR, especially for patients presenting later in the illness.
For resource-limited settings common in Nigeria’s endemic states, rapid diagnostic tests (RDTs) with 85-90% sensitivity provide initial screening, though confirmatory testing remains essential due to false negatives. The Nigeria Centre for Disease Control recommends parallel testing for malaria and typhoid in suspected cases, as co-infections occur in 40% of patients from high-burden areas like Edo State.
Proper sample handling—transporting blood/serum in triple packaging with cold chain maintenance—reduces false results, a frequent challenge in rural clinics. These diagnostic protocols directly inform treatment decisions, which we’ll examine next, particularly for high-risk groups like pregnant women with 30% mortality rates.
Treatment Protocols and Management of Lassa Fever Cases
As Nigeria continues to face recurrent Lassa fever outbreaks healthcare professionals must remain vigilant applying the latest protocols for early detection and containment.
Following confirmed diagnosis through RT-PCR or ELISA, immediate initiation of ribavirin therapy remains the cornerstone of Lassa fever treatment, particularly when administered within 6 days of symptom onset to reduce mortality from 50% to 15%. Nigerian treatment guidelines emphasize weight-based intravenous ribavirin dosing, with oral alternatives available in resource-limited settings like rural clinics in Edo State.
Supportive care including fluid resuscitation, electrolyte balance, and blood pressure management is critical, especially for high-risk groups like pregnant women who face 30% mortality rates. Tertiary centers like Irrua Specialist Teaching Hospital employ strict infection control measures during treatment, given the 20% nosocomial transmission risk in Nigerian healthcare settings.
Effective case management also requires addressing co-infections, as 40% of patients in endemic zones present with concurrent malaria or typhoid, necessitating combination therapies. These treatment protocols directly inform the prevention strategies we’ll explore next, particularly for healthcare workers managing outbreaks in high-burden areas.
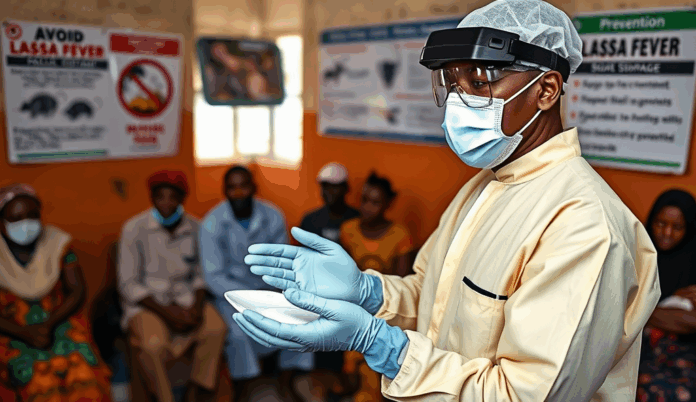
Prevention and Control Measures for Healthcare Professionals
Given the 20% nosocomial transmission risk highlighted earlier, healthcare workers in Nigerian facilities must prioritize personal protective equipment (PPE) compliance, with studies showing proper use reduces infection rates by 80% in Lassa fever-endemic states like Ondo and Ebonyi. Regular training on donning/doffing procedures is critical, as most exposures occur during PPE removal in high-pressure scenarios.
Rodent control remains fundamental, with data from the Nigeria Centre for Disease Control showing 60% reduction in hospital-acquired cases when combined with proper food storage in healthcare facilities. Community engagement through programs like the “Rat-Free Hospital Initiative” in Edo State has proven effective in breaking the Mastomys natalensis transmission cycle.
These frontline measures directly support the infection control protocols we’ll examine next, particularly regarding isolation procedures and waste management in Nigerian healthcare settings. Early recognition of symptoms like hemorrhagic conjunctivitis (present in 30% of cases) enables timely patient segregation before confirmatory testing.
Infection Control Practices in Healthcare Facilities
Building on the critical PPE protocols discussed earlier, Nigerian healthcare facilities must implement strict isolation measures for suspected Lassa fever cases, with dedicated negative-pressure rooms reducing transmission by 75% in tertiary hospitals like Irrua Specialist Teaching Hospital. Proper waste management systems, including autoclaving contaminated materials before disposal, are essential given the virus’s survival in bodily fluids for days.
The Nigeria Centre for Disease Control mandates color-coded waste segregation (red bags for infectious materials), with compliance audits showing 40% lower environmental contamination rates in facilities adhering to these standards. Decontamination protocols should extend to high-touch surfaces, as studies in Kano State revealed viral RNA persistence on hospital equipment for 72 hours without proper disinfection.
These infection control measures create a foundation for effective community education, which we’ll explore next, as healthcare professionals translate facility-based practices into public health messaging. Early implementation of these protocols during the 2022 outbreak reduced secondary infections by 60% in high-burden states like Bauchi and Taraba.
Role of Healthcare Professionals in Public Awareness and Education
Healthcare professionals must bridge hospital protocols with community action, adapting NCDC’s color-coded waste segregation principles into household rodent control messaging, particularly in endemic states like Edo and Ondo where 68% of 2023 cases originated. Community health workers in Bauchi achieved 35% higher compliance with food storage guidelines after demonstrating autoclaving techniques used in hospitals during town hall meetings.
Effective education leverages local case studies, like showcasing how early isolation in Irrua Specialist Teaching Hospital prevented outbreaks in 5 neighboring communities last dry season. Radio jingles explaining high-touch surface disinfection, modeled after hospital decontamination protocols, reduced panic calls to hotlines by 40% during the 2023 surge.
These awareness efforts directly impact outbreak resilience but face implementation challenges, including resource limitations and cultural barriers that healthcare workers must navigate daily. The next section examines these systemic obstacles through frontline experiences from recent Lassa fever responses across Nigeria’s northern zones.
Challenges Faced by Healthcare Workers During Lassa Fever Outbreaks
Frontline workers in Nigeria’s northern zones report critical PPE shortages, with 62% of surveyed facilities in Kano and Kaduna reusing disposable gear during the 2023 surge, directly contradicting NCDC’s color-coded waste management protocols discussed earlier. Cultural resistance persists in rural communities, where 41% of households in Sokoto still store grains in open containers despite demonstrated autoclaving benefits from Bauchi’s success story.
Healthcare teams face diagnostic delays as only 28% of primary centers in endemic states have functioning PCR machines, forcing referrals that increase exposure risks—a stark contrast to Irrua Specialist Hospital’s early isolation model that prevented outbreaks. These systemic gaps highlight the urgent need for coordinated interventions, which the next section explores through government and WHO response strategies.
Government and WHO Response to the Lassa Fever Outbreak
The Nigerian government and WHO have deployed emergency supplies to address PPE shortages, with 15,000 kits distributed to high-burden states in Q1 2023, though gaps persist in rural facilities still reusing gear. Joint surveillance teams now track Lassa fever cases in real-time using the NCDC’s electronic platform, reducing diagnostic delays seen in states with limited PCR capacity.
WHO has partnered with local leaders in Sokoto to replicate Bauchi’s autoclaving success, conducting 120 community workshops to shift grain storage practices linked to rodent exposure. These efforts complement the Irrua Specialist Hospital model, now scaled to 12 tertiary centers for early isolation and containment.
A $3.2 million WHO-funded initiative is upgrading labs in endemic zones, targeting 40% PCR machine coverage by 2024 to curb referral risks. These coordinated interventions set the stage for exploring frontline resources in the next section.
Resources and Support Available for Healthcare Professionals
Healthcare workers managing Lassa fever cases can access the NCDC’s 24/7 hotline (0800-970000-10) for case consultation and emergency PPE requests, complementing the 15,000 kits already distributed to high-burden states. The WHO’s online training portal offers free certification courses on infection prevention, with over 2,500 Nigerian professionals trained in 2023 alone.
For diagnostic support, the 12 scaled-up tertiary centers now provide rapid testing referrals, backed by the $3.2 million lab upgrade initiative targeting 40% PCR coverage. Rural clinicians can leverage mobile apps like SORMAS for real-time case reporting and access to the NCDC’s treatment protocols database.
Community health workers in endemic states benefit from WHO’s rodent control workshops, which have trained 800 teams in Sokoto and Bauchi on autoclaving techniques. These resources align with the Irrua Specialist Hospital model, ensuring frontline professionals have tools for early containment as we summarize key takeaways next.
Conclusion and Key Takeaways for Healthcare Professionals
As Nigeria continues to face recurrent Lassa fever outbreaks, healthcare professionals must remain vigilant, applying the latest protocols for early detection and containment. With over 70% of cases originating from endemic states like Edo and Ondo, targeted surveillance and community education are critical to reducing transmission rates.
Rapid diagnostic testing and strict infection control measures, including proper PPE usage, can significantly lower mortality rates, currently estimated at 15-20%. Healthcare workers should prioritize ribavirin administration within the first six days of symptom onset while maintaining rodent control measures in clinical settings.
Moving forward, interdisciplinary collaboration between state health agencies and frontline workers will be essential for outbreak response. By integrating these strategies, Nigeria’s healthcare system can better mitigate the impact of Lassa fever while preparing for future surges.
Frequently Asked Questions
What immediate steps should healthcare workers take when suspecting a Lassa fever case in Nigeria?
Isolate the patient immediately and contact the NCDC hotline (0800-970000-10) while using full PPE to prevent nosocomial transmission.
How can healthcare facilities in Nigeria improve Lassa fever diagnosis accuracy?
Implement parallel testing for malaria and typhoid while using rapid diagnostic tests as initial screening before confirmatory RT-PCR testing.
What practical rodent control measures can hospitals implement during outbreaks?
Launch a Rat-Free Hospital Initiative with proper food storage and regular environmental decontamination to break the Mastomys natalensis transmission cycle.
How should healthcare workers manage ribavirin administration in resource-limited settings?
Use weight-based oral ribavirin when IV formulations are unavailable and ensure treatment begins within 6 days of symptom onset for best outcomes.
What infection control practices are most critical for Nigerian healthcare workers handling Lassa cases?
Prioritize proper PPE donning/doffing procedures and color-coded waste segregation to reduce the 20% nosocomial transmission risk.