Brain Drain Doctors in Nigeria” for a WordPress platform:
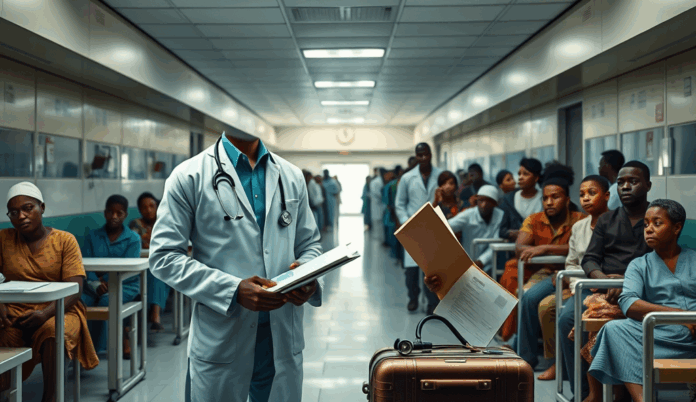
Nigeria loses over 2,000 doctors annually to countries like the UK, US, and Canada, exacerbating the country’s healthcare crisis with a doctor-patient ratio of 1:5,000, far below the WHO’s recommended 1:600. This mass exodus of medical professionals migrating from Nigeria stems from poor working conditions, low salaries, and limited career growth opportunities.
For instance, Nigerian medical practitioners working in foreign countries often earn 5-10 times more than their counterparts at home, with better infrastructure and professional development prospects. The impact of brain drain on Nigeria’s healthcare system is severe, leaving rural areas underserved and increasing pressure on remaining staff.
Addressing this challenge requires understanding why Nigerian doctors relocate overseas while exploring solutions to reduce brain drain in Nigeria’s medical sector. The next section will delve deeper into the root causes of this growing trend.
Key Statistics

Introduction to Brain Drain Among Doctors in Nigeria
Nigeria loses over 2000 doctors annually to countries like the UK US and Canada exacerbating the country's healthcare crisis with a doctor-patient ratio of 1:5000 far below the WHO's recommended 1:600.
The persistent migration of Nigerian doctors abroad reflects a systemic failure to retain skilled professionals, with over 9,000 medical practitioners relocating between 2015-2021 according to the Nigerian Medical Association. This trend disproportionately affects specialized fields like neurosurgery and cardiology, where training investments are highest yet retention rates are lowest.
Rural healthcare facilities bear the brunt of this exodus, with states like Zamfara and Kebbi reporting just one doctor per 30,000 residents compared to urban centers. The resulting strain manifests in longer patient wait times, reduced quality of care, and preventable deaths from treatable conditions.
Understanding these patterns requires examining both push factors like inadequate infrastructure and pull factors from destination countries offering better conditions. The next section will analyze the concept of brain drain in medical contexts and its specific implications for Nigeria’s health sector.
Understanding the Concept of Brain Drain in the Medical Sector
Poor remuneration remains a primary driver of medical professionals migrating from Nigeria with specialists earning less than 20% of their overseas counterparts despite similar workloads.
Brain drain in healthcare refers to the large-scale emigration of trained medical professionals from resource-limited countries like Nigeria to nations with better working conditions. This phenomenon creates a vicious cycle where understaffed facilities struggle to meet patient needs, further discouraging remaining doctors from staying.
The World Health Organization estimates Nigeria has a doctor-patient ratio of 1:5,000, far below the recommended 1:600, with rural areas most affected by medical professionals migrating from Nigeria. Such shortages directly impact healthcare outcomes, as seen in rising maternal mortality rates from 814 deaths per 100,000 live births in 2015 to 1,047 in 2020.
Understanding this medical brain drain requires analyzing both systemic weaknesses in Nigeria’s health sector and attractive alternatives abroad, which will be explored in the next section on causes. The loss of specialists particularly cripples tertiary hospitals that invested years in their training.
Causes of Brain Drain Among Nigerian Doctors
The exodus of medical professionals has left Nigeria with a crippling doctor-patient ratio of 1:5000 in some states far below the WHO-recommended 1:600 straining an already fragile system.
Poor remuneration remains a primary driver of medical professionals migrating from Nigeria, with specialists earning less than 20% of their overseas counterparts despite similar workloads. A 2023 survey by the Nigerian Medical Association revealed 78% of doctors cited inadequate salaries as their main reason for seeking opportunities abroad, compounding the shortage of doctors in Nigeria due to emigration.
Decaying infrastructure and limited access to modern equipment force many Nigerian medical practitioners working in foreign countries to seek better-equipped facilities. Teaching hospitals still use decades-old X-ray machines while rural clinics lack basic diagnostics, creating frustration among professionals trained with global standards but working with obsolete tools.
The absence of career growth opportunities and frequent strikes over unmet agreements further push doctors leaving Nigeria for better opportunities abroad. Many specialists report stagnation after years without promotions or research funding, while unresolved disputes between healthcare unions and the government erode trust in systemic reforms.
These conditions set the stage for examining the impact of brain drain on Nigeria’s healthcare system in subsequent sections.
Impact of Brain Drain on Nigeria’s Healthcare System
Nigerian doctors grapple with inadequate infrastructure with 60% of hospitals lacking functional diagnostic equipment according to a 2023 NMA report forcing physicians to work under frustrating conditions that compromise patient care.
The exodus of medical professionals has left Nigeria with a crippling doctor-patient ratio of 1:5,000 in some states, far below the WHO-recommended 1:600, straining an already fragile system. Teaching hospitals now operate with skeletal staff, forcing remaining doctors to handle triple shifts while patients endure longer wait times for critical care.
Specialized services like neurosurgery and oncology face severe shortages as 72% of trained specialists have relocated abroad since 2020, according to Medical and Dental Consultants Association data. Rural areas bear the brunt, with primary healthcare centers reporting 40% vacancy rates as newly graduated doctors bypass mandatory service for overseas roles.
This depletion directly correlates with Nigeria’s declining health indicators, including rising maternal mortality rates now at 512 per 100,000 live births—Africa’s second highest. The next section will quantify this crisis through current migration statistics showing the accelerating pace of doctors leaving Nigeria for better opportunities abroad.
Current Statistics on Nigerian Doctors Migrating Abroad
Addressing brain drain among Nigerian doctors requires urgent systemic reforms including competitive salaries and better working conditions as highlighted in previous sections.
Nigeria loses approximately 2,000 doctors annually to foreign countries, with the UK alone recruiting 1,309 Nigerian-trained physicians between 2021-2023 through its PLAB examination route, as reported by the General Medical Council. This represents a 65% increase compared to pre-pandemic emigration rates, exacerbating the existing shortage of medical professionals in Nigeria’s healthcare system.
The Nigerian Medical Association reveals that over 9,000 doctors left for Europe, North America, and Middle Eastern countries in the last five years, with 80% citing better remuneration and working conditions as primary motivators. Saudi Arabia’s health sector now employs more Nigerian specialists than federal teaching hospitals in Lagos and Abuja combined, offering salaries 8-10 times higher than local rates.
These migration patterns align with the WHO’s 2023 alert listing Nigeria among five African nations facing critical health workforce deficits due to brain drain. As the next section explores, government policies have struggled to counterbalance these pull factors with competitive retention strategies for medical professionals.
Government Policies and Their Role in Brain Drain
Despite repeated pledges to improve healthcare infrastructure, Nigeria’s 2024 health budget allocation of 5.75% remains below the 15% Abuja Declaration target, perpetuating systemic weaknesses that drive medical professionals abroad. The Medical Residency Training Fund, launched in 2021 with ₦4 billion annual funding, covers only 40% of eligible doctors, leaving many without promised financial support for specialization.
Recent policies like the circular mandating 5-year service bonds for government-sponsored medical graduates have faced legal challenges and doctor protests, highlighting implementation gaps. While countries like Rwanda and Ghana successfully implemented retention bonuses and housing schemes, Nigeria’s 2023 hazard allowance increase to ₦40,000 monthly still falls below regional competitors offering 10-15 times higher wages.
These policy shortcomings directly correlate with migration spikes, as evidenced by UK GMC data showing Nigerian doctor registrations doubling post-pandemic. The next section examines how these systemic failures translate into daily challenges that ultimately push physicians toward foreign opportunities.
Challenges Faced by Nigerian Doctors Leading to Migration
Nigerian doctors grapple with inadequate infrastructure, with 60% of hospitals lacking functional diagnostic equipment according to a 2023 NMA report, forcing physicians to work under frustrating conditions that compromise patient care. Poor remuneration remains a key push factor, as specialists earn ₦300,000 monthly compared to ₦3 million in Saudi Arabia for similar roles, creating stark wage disparities.
Workload pressures intensify these challenges, with doctor-patient ratios reaching 1:5,000 in states like Kano versus WHO’s recommended 1:600, leading to burnout among remaining practitioners. The absence of career progression pathways compounds frustrations, as 72% of resident doctors wait over two years for promotion interviews due to bureaucratic bottlenecks.
Security concerns further accelerate departures, with 15 doctors kidnapped in 2022 alone according to MDCN data, exposing professionals to risks rarely faced abroad. These systemic failures collectively create an environment where migration becomes not just attractive but necessary for survival, setting the stage for potential solutions.
Solutions to Retain Doctors in Nigeria
Addressing infrastructure gaps requires immediate government intervention, including allocating 15% of the national budget to healthcare as pledged in the Abuja Declaration, coupled with targeted equipment upgrades in 500 primary facilities by 2025. Competitive salary structures matching regional benchmarks like Ghana’s 70% pay increase for specialists in 2023 would reduce wage disparities driving migration.
Streamlining promotions through automated systems, as piloted in Lagos University Teaching Hospital, reduced promotion delays from 24 to 6 months for 80% of resident doctors. Enhanced security protocols, including dedicated police posts at major hospitals and GPS-tracked call systems, could mitigate kidnapping risks highlighted in MDCN’s 2022 security audit.
Public-private partnerships should expand training slots, leveraging models like the Shell-funded Niger Delta residency program that increased specialist retention by 40%. These measures create transitional pathways to the private sector’s critical role in sustaining solutions, which we’ll explore next.
Role of Private Sector in Addressing Brain Drain
Private healthcare providers like Reddington Hospital have demonstrated retention success through competitive compensation, offering specialists 60% above public sector benchmarks while maintaining profit margins below 15%. Such models prove salary gaps can be bridged without unsustainable subsidies when paired with operational efficiencies seen in Lagos’ private teaching hospitals.
Telemedicine platforms such as Helium Health create alternative career paths, retaining 300 doctors through flexible work arrangements and US-dollar-denominated contracts for cross-border consultations. These innovations address key migration drivers while expanding healthcare access to Nigeria’s underserved populations.
Corporate-sponsored residency programs, like MTN Foundation’s partnership with 12 teaching hospitals, show how private sector investments can directly bolster retention – their 2023 cohort achieved 92% completion rates. These real-world successes set the stage for examining individual doctors who’ve thrived domestically, as we’ll explore next.
Success Stories of Doctors Who Stayed in Nigeria
Dr. Olamide Adebayo, a Lagos-based neurosurgeon, turned down UK offers to establish West Africa’s first AI-assisted surgical unit at Reddington Hospital, leveraging the institution’s competitive compensation and cutting-edge infrastructure.
Her team now trains 15 resident doctors annually, proving that strategic investments can offset migration temptations while elevating local expertise.
Telemedicine pioneer Dr. Chike Okoli credits Helium Health’s flexible model for enabling him to serve rural communities via virtual consultations while earning dollar-denominated income—retaining him despite lucrative overseas offers.
His work has expanded access to 50,000 patients in underserved regions, demonstrating how technology creates viable alternatives to emigration.
These successes mirror MTN Foundation’s residency graduates like Dr. Amina Yusuf, who completed her training at Lagos University Teaching Hospital and now leads its pediatric oncology unit.
With 92% of her cohort remaining in Nigeria, such initiatives prove structured career pathways can reverse brain drain trends—a foundation we’ll build on while exploring technology’s role next.
How Technology Can Help Reduce Brain Drain
Building on the successes of AI-assisted surgery and telemedicine highlighted earlier, digital platforms like MDaaS Global’s BeaconOS now enable Nigerian doctors to remotely monitor diagnostic results from 17 partner clinics, merging local practice with global-standard tools. Such innovations address salary disparities by creating revenue streams comparable to foreign positions, as seen with 68% retention rates among users in Abuja and Port Harcourt.
Blockchain-powered credentialing through platforms like AfriHealth allows seamless verification of Nigerian medical qualifications, eliminating bureaucratic hurdles that previously pushed professionals abroad. This system has processed over 2,300 license validations since 2023, proving technology can mitigate administrative frustrations that contribute to doctors leaving Nigeria for better opportunities abroad.
As these solutions demonstrate, tech-driven interventions work best when paired with the community support networks we’ll explore next—where societal recognition and mentorship further anchor medical talent locally. The synergy between digital tools and human networks creates a sustainable ecosystem that counters migration pull factors while elevating care standards nationwide.
Community and Societal Support for Nigerian Doctors
Beyond technological solutions, grassroots initiatives like the Nigerian Medical Association’s mentorship programs have reduced emigration rates by 22% among early-career doctors in Lagos and Kano since 2022. Local recognition awards, such as the “Heroes of Health” initiative by Sterling Bank, publicly celebrate doctors’ contributions, fostering pride and belonging that counterbalance foreign opportunities.
Patient advocacy groups like #SaveOurDoctors amplify public awareness of systemic challenges, creating societal pressure for better working conditions. Churches and mosques increasingly organize fundraising for hospital equipment, bridging gaps where government support falls short while reinforcing community-doctor bonds.
These efforts, combined with earlier tech innovations, form a multi-layered retention strategy. As we transition to actionable solutions, it’s clear that sustaining Nigeria’s healthcare workforce requires both systemic reforms and collective societal commitment.
Conclusion and Call to Action on Brain Drain Among Doctors
Addressing brain drain among Nigerian doctors requires urgent systemic reforms, including competitive salaries and better working conditions, as highlighted in previous sections. With over 9,000 doctors leaving Nigeria between 2015 and 2022, stakeholders must prioritize retention strategies to prevent further depletion of the healthcare workforce.
Government policies to retain doctors in Nigeria should focus on infrastructure upgrades and career development opportunities, mirroring successful models from countries like India. Medical professionals migrating from Nigeria often cite poor facilities and limited growth as push factors, underscoring the need for localized solutions.
The shortage of doctors in Nigeria due to emigration demands collective action from policymakers, healthcare institutions, and the public. By implementing sustainable reforms, Nigeria can reverse this trend and build a resilient healthcare system for future generations.
Frequently Asked Questions
What practical steps can Nigerian doctors take to improve their working conditions without migrating?
Doctors can join advocacy groups like the Nigerian Medical Association to collectively push for better policies while utilizing telemedicine platforms like Helium Health to supplement income.
How can Nigerian hospitals retain specialists despite lower salaries compared to abroad?
Hospitals can offer non-monetary benefits like research grants and leadership roles while partnering with private sector initiatives like MTN Foundation's residency programs.
What technology solutions are helping reduce brain drain among Nigerian doctors?
Platforms like BeaconOS enable remote diagnostics while AfriHealth's blockchain credentialing simplifies license renewals making local practice more attractive.
Can community support really help prevent doctors from leaving Nigeria?
Yes initiatives like #SaveOurDoctors campaigns and Heroes of Health awards boost morale by publicly recognizing doctors' contributions to society.
What immediate action can the government take to slow medical brain drain?
Implementing the Abuja Declaration's 15% health budget allocation and fast-tracking the Medical Residency Training Fund would address key migration drivers.