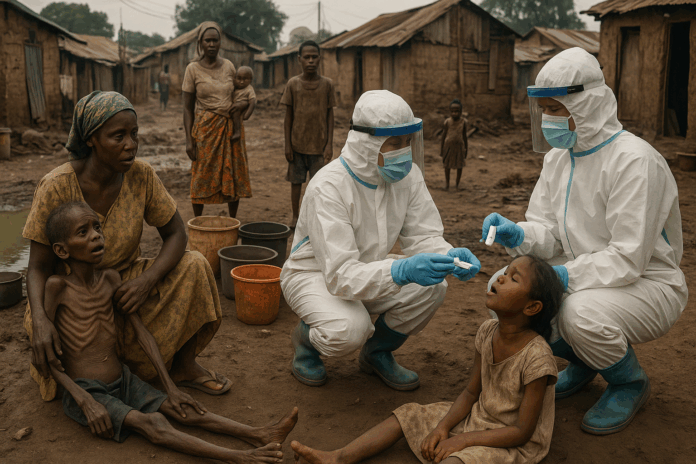
A silent tsunami of disease and deprivation is engulfing Nigeria. As the rainy season intensifies in July 2025, 4.93 million Nigerians desperately need emergency health assistance – equivalent to the entire population of Ireland left without basic medical care. This staggering figure represents vulnerable children, pregnant women, the elderly, and displaced populations caught in a perfect storm of surging cholera outbreaks, escalating malaria transmission, and protracted conflict. Rivers State has already reported cholera claiming 9 lives in January 2025 alone, while nationwide floods have transformed communities into disease incubators. With clinics shuttered, vaccines depleted, and funding evaporating, the very concept of humanitarian health access – the ability to reach and deliver life-saving care to those in crisis – is collapsing. This is the anatomy of a health emergency threatening to erase a generation.
Anatomy of a Crisis – Drivers Collapsing Health Access
Conflict’s Shattering Impact
Fifteen years of relentless violence in Borno, Adamawa, and Yobe states have displaced 2.3 million people, trapping communities without healthcare access as conflict tactics increasingly target civilians. The consequences are brutal: USAID-funded health facilities in Borno – once serving 300 patients daily – have abruptly shut down, eliminating free malaria drugs and mosquito nets for vulnerable communities. Nurse Musa Adamu Ibrahim describes abandoned clinics creating “medical deserts” where families must walk for days to find care: “People with resources might find drugs… but the poorest in remote areas? Their children will die.” Overcrowded camps like Borno’s 1.7 million internally displaced persons sites become cholera breeding grounds, with sanitation systems destroyed by fighting.
Climate Shocks as Crisis Multipliers
Nigeria’s 2024 floods – impacting 3 million people and destroying 226,000 homes – contaminated water sources and triggered cholera outbreaks that killed 378 Nigerians by October. The climate-health connection is vicious: stagnant floodwaters create ideal mosquito breeding conditions just as malnutrition weakens immune systems. Fatima Kunduli, a laid-off Borno health worker, reported treating 60 children daily for malaria and malnutrition before her clinic closed. Submerged farmland caused massive crop losses, decimating food security for 13 million people and leaving children too weak to fight cholera. Tropical Cyclone Chido’s December 2024 destruction of regional water infrastructure signals climate threats amplifying Nigeria’s vulnerability.
| Crisis Driver | Human Impact | Health Consequence |
|---|---|---|
| 2024 Flooding | 3 million affected | 14,000+ cholera cases |
| BAY Conflict | 2.3 million displaced | 70% health services non-functional |
| 2025 Rains | Rising malaria risk | Critical bed net shortage |
System Fragility & Disease Surges
Nigeria’s health infrastructure is crumbling where it’s needed most: between January-September 2024, Nigeria recorded 11,000 suspected cholera cases and 359 deaths across 36 states – a 300% increase from 2023. The 2025 outbreak continues with 1,214 cases and 28 deaths by March. With seasonal chemoprevention programs defunded and clinics closed, malaria deaths could surpass 2024’s 30% global share representing over 180,000 Nigerian deaths. Thirty-one percent of health facilities in conflict zones are non-functional, creating treatment gaps where mobile clinics report one nurse for every 5,000 internally displaced persons.
Human Face of the Statistics – Who Suffers Most?
Children: The Invisible Casualties
A nutritional Armageddon unfolds: UNICEF projects 2.6 million under-five children in northeast Nigeria will face acute malnutrition in 2025 – including 1 million with severe acute malnutrition, doubling 2024’s catastrophic figures. The deadly math reveals that severely malnourished children are 9-12 times more likely to die from cholera due to compromised immunity. In flood-ravaged Maiduguri, health promoters found infants dying from dehydration before reaching shuttered clinics. Save the Children documented children dying during hours-long walks to cholera treatment in South Sudan – a fate now threatening Nigerian children as clinics close.
Women: Bearing the Brunt
Pregnant women in Borno face a maternal health nightmare: only 33% deliver with skilled attendants despite 67% attending antenatal clinics, creating deadly gaps when complications arise. Flood displacement camps report surging sexual violence against women and girls, with protection services crippled by funding cuts. As Nigeria’s Health Minister admits: “No pregnancy should be considered routine, and no maternal death is acceptable – each loss is one too many.”
The Displaced: Trapped in Medical Deserts
For Nigeria’s 2.3 million internally displaced persons, healthcare is a phantom promise: 868,000 returnees lack basic health services after returning to destroyed communities. Mobile units treat cholera patients on floors amid bed shortages. “Having a document to quickly refer to is invaluable,” admits Modu Kyari, a Borno health promoter, describing makeshift cholera response guides. Despite Borno receiving 600,000 cholera vaccines in 2024, distribution gaps leave displacement camps unprotected against new outbreaks.
Roadblocks to Lifesaving Care – Why Health Access is Failing
Funding Catastrophe
The lifeline is severed: the 2025 Borno, Adamawa, and Yobe Lean Season Plan faces a $159 million funding gap for health and nutrition interventions despite 4.6 million facing emergency hunger. USAID’s exit collapsed malaria programs across Africa. In Mali, life-saving childhood chemoprevention drugs sit stranded in warehouses without distribution networks. With Nigeria’s currency losing 70% value against the dollar, common medicines like paracetamol become luxury goods in camps where refugees protest ration cuts.
Vaccine & Supply Chain Failures
Global systems are failing Nigeria: the global oral cholera vaccine stockpile stands at 3.6 million doses – dangerously below the 5-million-dose emergency threshold. Seasonal malaria chemoprevention for children – crucial during rains – has stalled without coordination funds, creating coverage gaps in multiple provinces now threatening Nigeria. Even available supplies fail to reach clinics as communities report waste disposal challenges that sabotage cholera prevention despite education efforts.
Systemic Neglect & Governance
Decades of underinvestment fuel the crisis: cholera thrives where “inadequate sanitation and hygiene” persist – a chronic condition in 40% of Nigerian communities. Remote areas face critical health worker shortages. Clinics that trained staff on new maternal protocols now lack personnel to implement them. As health officials stress: “We must address underlying drivers through a unified approach” – yet cholera, malaria, and nutrition programs operate in silos.
Blueprint for Survival – Scaling Humanitarian Health Access
Immediate Lifesaving Priorities
We need battlefield triage tactics: deploy mobile units combining water purification tabs, oral rehydration stations, and ready-to-use therapeutic foods. In flood-ravaged Maiduguri, cholera education guides helped health workers deliver unified prevention messaging. Train community health workers to run “mini-clinics” in displacement camps for cholera screening, malaria testing, and severe malnutrition identification using telemedicine backup. Nigeria’s new safer birth protocols show this works when properly resourced.
| Disease | Immediate Action | Access Solution |
|---|---|---|
| Cholera | Community rehydration corners + IV fluid stations | Bypasses clinic distance |
| Malaria | Door-to-door bed net distribution + village testing kits | Overcomes medication shortages |
| Severe Acute Malnutrition | Mobile treatment units with therapeutic foods | Reaches children in medical deserts |
Building Resilience Through Systems
Stop-gap measures aren’t enough: invest in borehole rehabilitation and water monitoring. Surveys of 16,000 Nigerians revealed that trusted health educators are key to ending open defecation – a primary cholera driver. Train community volunteers in epidemic surveillance using simplified tools that trigger pre-positioned supplies. Nigeria’s new compact with state governors could enable this if funded. Scale Nigeria’s free emergency obstetric care initiative beyond current facilities using health sector renewal programs.
Advocacy & Resource Mobilization
The world must wake up: bridge the $159 million gap for lean season health and nutrition aid targeting 2 million highest-risk people. Leverage Nigeria’s petroleum industry funds for clinic rehabilitation – transforming oil wealth into health access. Demand wealthy nations replenish the cholera vaccine stockpile beyond the emergency 5-million-dose threshold.
The Hourglass is Empty – A Call for Concerted Action
Nigeria’s humanitarian health access crisis – epitomized by 4.9 million needing urgent care – is not destiny but policy failure. As cholera kills in Rivers State, malaria ravages malnourished children in Borno, and floods destroy clinics, band-aid solutions won’t suffice. Sustainable health access demands three shifts: combine cholera, malaria, and nutrition responses into single survival packages delivered door-to-door; empower state governments to lead clinic rehabilitation; treat water access as a human right – drilling boreholes is cheaper than cholera treatment.
The hundreds of cholera deaths across Africa are not just numbers – they are mothers like Fatima Kunduli who once saved children before her clinic closed, farmers who fed communities before floods drowned their fields, and babies whose malnutrition diagnosis became a death sentence when funding vanished. We must act before the next rain, the next outbreak, the next war erases more futures. The lifeline begins with clean water, continues with nourished children, and ends with clinics that never close their doors.
Crisis Snapshot: Nigeria’s Health Emergency
• 4.93M needing emergency health access
• 1M children with severe acute malnutrition – double 2024’s crisis
• $159M funding gap for life-saving health interventions
• 70% currency devaluation making medicines unaffordable
• 3.6M global cholera vaccine doses available – below emergency threshold
Critical Timeline
Jan 2024 ▶ Cholera outbreaks begin across 36 states
Oct 2024 ▶ Devastating floods affect 3M people, contaminate water
Jan 2025 ▶ Rivers State cholera outbreak claims 9 lives
Apr 2025 ▶ Funding cuts force clinic closures across Borno
May 2025 ▶ Global cholera vaccine stockpile drops to 3.6M doses
Jul 2025 ▶ Rainy season escalates cholera and malaria risks